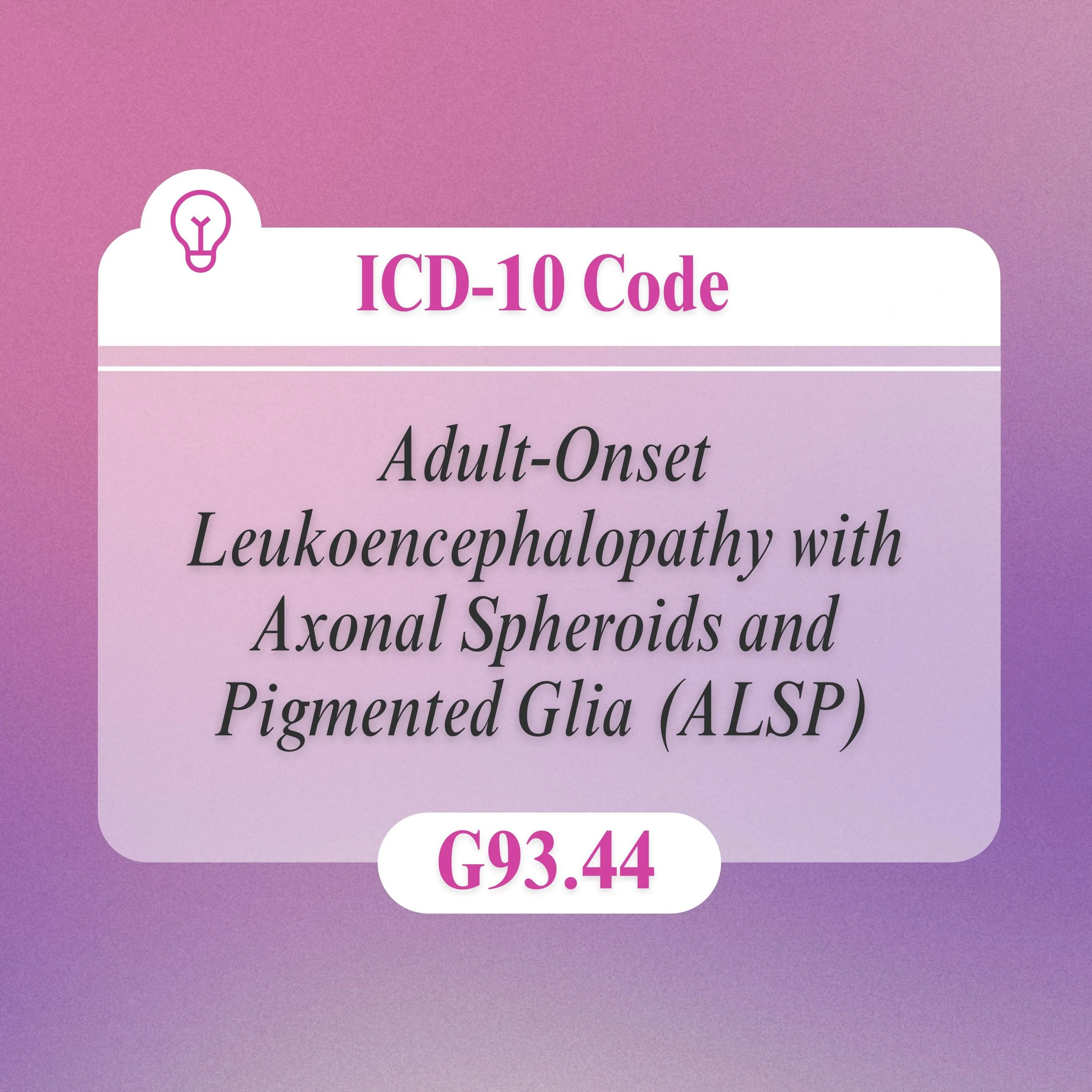
Diagnosis
ALSP can be difficult to diagnose due to the varied presentation of symptoms. Signs that may lead doctors to order additional testing include family history, early onset of cognitive and movement-related symptoms (before age 60), and brain imaging that shows white matter lesions and other deterioration. ALSP is commonly misdiagnosed because many symptoms overlap with other types of leukodystrophies and neurological disorders, including frontotemporal dementias, multiple sclerosis, Parkinson’s disease and early onset Alzheimer’s disease.
Genetic Testing
Genetic testing to identify the CSF1R or AARS1/AARS2 gene variant can provide a definitive diagnosis for ALSP.
Other tests your doctor may order to rule out other conditions include:
Electromyogram (EMG). A needle is inserted through the skin into various muscles. The test records the electrical activity of the muscles when they contract and when they’re at rest. This can determine if there is a problem with the muscles or nerves.
Nerve conduction study. This study measures your nerves’ ability to send impulses to muscles in different areas of the body. This test can determine if you have nerve damage. EMG and nerve conduction studies are almost always done together.
MRI. Using radio waves and a powerful magnetic field, an MRI produces detailed images of the brain and spinal cord. An MRI can reveal spinal cord tumors, herniated disks in the neck or other conditions that might be causing your symptoms. The highest resolution cameras may sometimes see ALSP changes themselves.
Blood and urine tests. Analyzing samples of your blood and urine in the laboratory might help eliminate other possible causes of your symptoms. Serum neurofilament light levels, which are measured from blood samples, are generally high in people with ALSP. The test can help make a diagnosis early in the disease.
Spinal tap, known as a lumbar puncture. This involves removing a sample of spinal fluid for laboratory testing. Spinal fluid is removed using a small needle inserted between two bones in the lower back. The spinal fluid contains potential ALSP biomarkers.
Treatment
There are currently no FDA approved treatments for ALSP. Medications can be used to help manage and relieve symptoms. Your healthcare team will work together to select the right therapies and treatments for your specific symptoms.
Based on the current understanding of ALSP, medical researchers and biotechnology companies are conducting studies and clinical trials as they work toward treatment and cure options.
10,000: ESTIMATED NUMBER OF ALSP CASES IN THE UNITED STATES
●
43: AVERAGE AGE AT DIAGNOSIS
●
75%: PERCENT OF ALSP PATIENTS MISDIAGNOSED OR UNDIAGNOSED
●
8 YEARS: AVERAGE LIFE EXPECTANCY AFTER SYMPTOM ONSET
●
10,000: ESTIMATED NUMBER OF ALSP CASES IN THE UNITED STATES ● 43: AVERAGE AGE AT DIAGNOSIS ● 75%: PERCENT OF ALSP PATIENTS MISDIAGNOSED OR UNDIAGNOSED ● 8 YEARS: AVERAGE LIFE EXPECTANCY AFTER SYMPTOM ONSET ●
Sisters’ Hope Foundation has partnered with AspireCURES to provide the latest information on research studies and clinical trials. Register with AspireCURES to be matched with eligible upcoming opportunities and to receive updates from the ALSP scientific community.

Clinical Trials & Observational Studies
Therapies
When ALSP affects your ability to speak, move, and complete activities of daily living, therapies may help.
Physical therapy: A physical therapist can address pain, walking, mobility, and equipment needs that help you stay independent. Practicing low-impact exercises can help maintain your cardiovascular fitness, muscle strength and range of motion for as long as possible. Regular exercise also can help improve your sense of well-being. Appropriate stretching can help prevent pain and help your muscles function at their best.
A physical therapist also can help you overcome weakness by using a brace, walker or wheelchair. The therapist might suggest devices such as ramps that make it easier for you to get around.Occupational therapy: An occupational therapist can help you find ways to remain independent through the use of adaptive equipment that can help you perform activities such as dressing, grooming, eating and bathing. An occupational therapist also can help you modify your home to allow accessibility if you have trouble walking safely.
Speech therapy: A speech therapist can teach you adaptive techniques to make your speech more understandable. Speech therapists also can help you find other ways to communicate. These may include using a smart phone app, alphabet board, or pen and paper. Ask your therapist about the possibility of recording your own voice to be used by a text-to-speech application.
Alternative therapies: These may include neurologic music therapy to improve brain function, motor skills, cognition and speech; aquatic (water) therapy to reduce pain, relieve joint pressure and reduce swelling; red light therapy to reduce inflammation, release tension and improve sleep.
Nutritional support: Your team typically works with you and your family members to ensure you are eating foods that are easier to swallow and meet your nutritional needs.
Psychological and social support: Your team might include a social worker to help with financial issues, insurance, getting equipment and paying for devices you need. Psychologists, social workers and others may provide emotional support for you and your family.